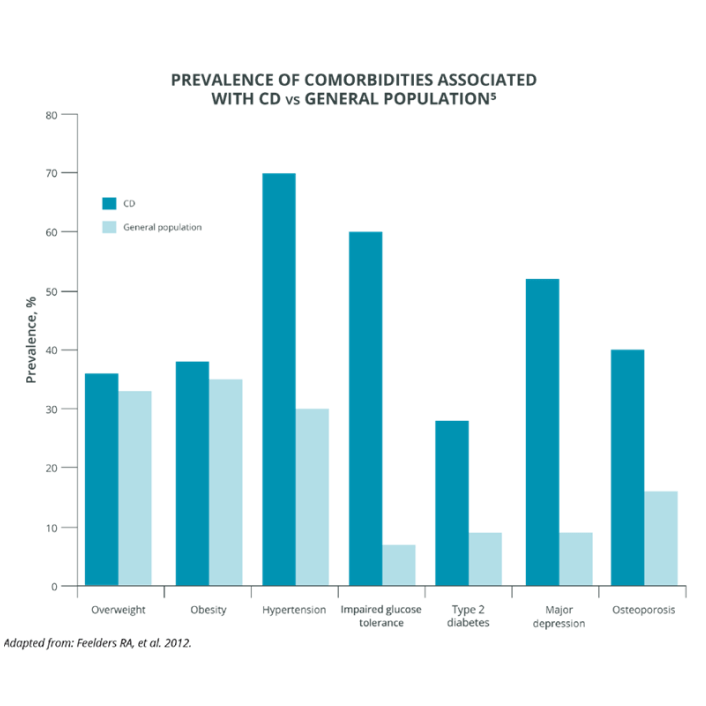
Sharma ST, Nieman LK, Feelders RA. Cushing’s syndrome: epidemiology and developments in disease management. Clin Epidemiol. 2015;17(7):281-293. doi:10.2147/CLEP.S44336 2. Lonser RR, Nieman L, Oldfield EH. Cushing’s disease: pathobiology, diagnosis, and management. J Neurosurg. 2017;126(2):404-417. doi:10.3171/2016.1.JNS152119 3. Giuffrida G, Crisafulli S, Ferraù F, et al. Global Cushing's disease epidemiology: a systematic review and meta-analysis of observational studies. Endocrinol Invest. 2022;45(6):1235-1246. doi:10.1007/s40618-022-01754-1 4. Nishioka H, Yamada S. Cushing's disease. Clin Med. 2019;8(11):1951. doi:10.3390/jcm8111951 5. Feelders RA, Pulgar SJ. Kempel A, Pereira AM. The burden of Cushing's disease: clinical and health-related quality of life aspects. Eur J Endocrinol. 2012;167(3):311-326. doi:10.1530/EJE-11-1095 6. Pivonello R, De Leo M, Cozzolino A, Colao A. The Treatment of Cushing's Disease. Endocr Rev. 2015 Aug;36(4):385-486. doi:10.1210/er.2013-1048 7. Nieman LK, Biller BMK, Findling JW. et al. Treatment of Cushing's syndrome: an Endocrine Society clinical practice guideline. Endocrine. 2015;100(8):2807-2831. doi:10.1210/jc.2015-1818 8. Fleseriu M, Auchus R, Bancos I, et al. Consensus on diagnosis and management of Cushing's disease: a guideline update. Lancet Diabetes Endocrinol. 2021;9(12):847-875. doi:10.1016/S2213-8587(21)00235-7 9. Dekkers OM, Biermasz NR, Pereira AM, et al. Mortality in patients treated for Cushing's disease is increased, compared with patients treated for nonfunctioning pituitary macroadenoma. J Clin Endocrinol Metab. 2007;92(3):976-981. doi:10.1210/jc.2006-2112 10. Lacroix A, Feelders RA, Stratakis CA, Nieman LK. Cushing's syndrome. Lancet. 2015;386(9996):913-927. doi:10.1016/S0140-6736(14)61375-1 11. Fleseriu M, Castinetti F. Updates on the role of adrenal steroidogenesis inhibitors in Cushing’s syndrome: a focus on novel therapies. Pituitary. 2016;19(6):643-653. doi:10.1007/s11102-016-0742-1 12. Dekkers OM, Horváth-Puhó E, Jørgensen JOL, et al. Multisystem morbidity and mortality in Cushing’s syndrome: a cohort study. J Clin Endocrinol Metab. 2013;98(6):2277-2284. doi:10.1210/jc.2012-3582 13. van Haalen FM, Broersen LHA, Jørgensen JO, Pereira AM, Dekkers OM. Management of endocrine disease: Mortality remains increased in Cushing’s disease despite biochemical remission: a systematic review and meta-analysis. Eur J Endocrinol. 2015;172(4):R143-R149. doi:10.1530/EJE-14-0556